Expert Advice On How To Cure Bacterial Vaginosis Overview of Bacterial Vaginosis
The Centers for Disease Control and Prevention (CDC) estimate that bacterial vaginosis (BV) affects over 21 million women in the US each year and is a common vaginal illness. When the good and bad bacteria in the vagina are out of balance, this disease develops. Vaginal discharge and a foul odor are common symptoms of BV.
Although a bacterial vaginosis (BV) is typically less painful than a yeast infection, if treatment is not received, BV can have more severe outcomes. These can include lower fertility, early labor, and a higher chance of contracting specific sexually transmitted infections (STDs). The dissatisfaction experienced by those afflicted is increased by the condition’s well-known tendency to return even after antibiotic therapy.
Thankfully, there are now practical over-the-counter treatments and lifestyle modifications that promote a healthy vaginal flora. These tactics can help control BV and stop flare-ups in the future, either by alone or in combination with traditional therapies.

In brief
The most prevalent vaginal illness among women who are of reproductive age is bacterial vaginosis (BV). It happens when there are more hazardous bacteria in the vagina than helpful bacteria.
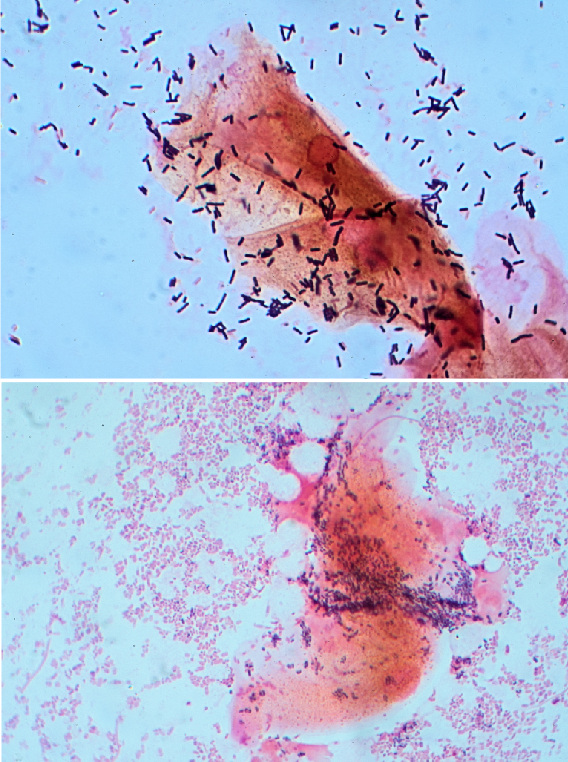
Causes and Symptoms of Bacterial Vaginosis (BV): BV is caused by a decrease in Lactobacillus bacteria in the vagina, which promotes the growth of anaerobic bacteria such as Gardnerella vaginalis. Although the precise etiology of BV is unknown, a number of variables can raise one’s chance of contracting the illness.
Anything that disturbs the vagina’s natural ecological environment might cause bacterial vaginosis (BV), according to Felice Gersh, M.D., OB/GYN, founder and director of the Integrative Medical Group of Irvine. This include engaging in sexual activity, douching, taking antibiotics, using spermicides and lubricants, and utilizing intrauterine devices (IUDs) or other forms of contraception. Furthermore, the proliferation of undesirable bacteria in the vaginal microbiome might be encouraged by anything that weakens immune function.
Vaginal health is influenced by your gut health as well. Recurrent BV is frequently associated with gut microbiota health, according to functional medicine gynecologist Wendie Trubow, M.D.
Variations exist in BV symptoms, and approximately 84% of women may not exhibit any symptoms at all. Those who do, however, have symptoms could observe:
a thin vaginal discharge that is fluid and white, yellowish, or gray.
A strong smell, particularly after intercourse, of fish
Vaginal pain, itchiness, or burning
burning when having a urinal
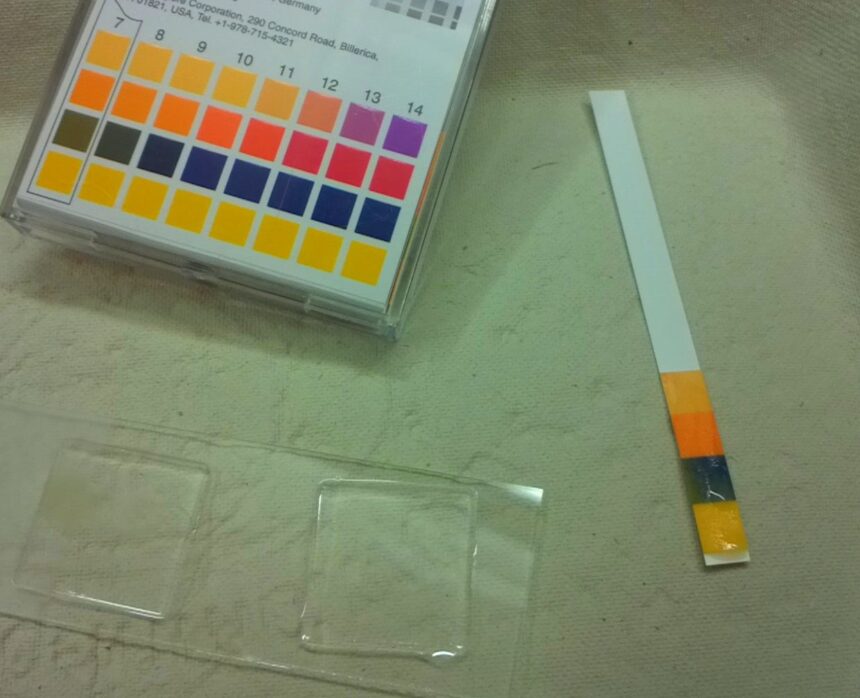
These symptoms are frequently used by doctors to identify BV; occasionally, a vaginal pH test is also used. A typical indicator of BV is a vaginal pH of 4.5 or above.
In conclusion, BV happens when the number of anaerobic bacteria in the vagina increases while Lactobacillus bacteria decreases. A strong fishy smell, a thin, yellowish discharge, or burning in the vagina are possible symptoms.
What Separates a Yeast Infection from a BV
Yeast infections and bacterial vaginosis are often confused by women, but it’s important to know the difference between the two since they need distinct care. Trubow claims that severe itching, a yeasty odor, and a thick, curd-like discharge are typical symptoms of yeast infections. The discharge from BV, on the other hand, is typically thinner, watery, and smells fishy.
An overabundance of yeast—specifically, Candida albicans—in the vagina results in a yeast infection. This can frequently happen after taking antibiotics, and it’s occasionally connected to eating refined carbohydrates and simple sugars.
Antibiotics like metronidazole or clindamycin are commonly used in the conventional treatment of bacterial vaginosis (BV), whereas fluconazole is an antifungal medicine used to treat yeast infections. Natural methods can also be used to treat these problems in order to lessen symptoms and lower the chance of recurrence.
In summary, an overgrowth of Candida albicans causes a yeast infection, whereas a bacterial imbalance causes BV. Symptoms vary; thick discharge and severe itching are signs of yeast infections, while thinner discharge and a fishy odor are signs of bacterial vaginosis.
Natural Solutions and Medical Advice for Bacterial Vaginosis Relief
Home Treatments for Viral Hemorrhage (Plus One to Ignore)
Despite receiving antibiotics, BV frequently returns three to twelve months later. Reducing recurrence and managing BV are possible with natural home treatments. Nonetheless, it’s crucial to speak with your physician before beginning any at-home treatments.
1 Daily Probiotic Supplements: Good gut health can positively impact the bacteria in your vagina. Probiotics assist in promoting the health of your gut microbiome. In addition to mentioning the benefits of utilizing oral supplements and vaginal suppositories, Trubow recommends probiotics, especially Lactobacillus strains. Bactobacillus acidophilus, Lactobacillus rhamnosus GR-1, and Lactobacillus fermentum RC-14 can be consumed at a dose of at least 10 billion CFU per day for two months in order to treat and prevent bacterial vaginosis (BV).
2 A Diet High in Nutrients: The vaginal microbiota may be impacted by a diet high in foods that are good for the gut. Include a range of plant foods high in fiber, as well as probiotic foods like kefir, yogurt, kimchi, and raw sauerkraut. It can also be beneficial to address systemic imbalances and food allergies.
3. Boric Acid Suppositories: For more than a century, boric acid has been used to treat BV. It comes in vaginally inserted capsule form; it is not meant to be swallowed. Trubow suggests using one suppository daily for ten days of treatment. In addition to having bacteriostatic, antiviral, and antifungal qualities, boric acid aids in restoring the pH balance of the vagina.
4.Tea Tree Oil Suppositories: Containing good Lactobacillus bacteria, tea tree oil has antibacterial qualities that allow it to specifically target bacteria that cause BV. Trubow suggests using tea tree oil suppositories every night for a period of six nights.
5. Supplements with Garlic: Garlic has strong antimicrobial qualities. Supplemental garlic was found to be equally efficient in treating bacterial vaginosis (BV) as metronidazole, but with less adverse effects (2014). For seven days, the participants took two 500 mg tablets of garlic twice a day.
6. Wear Breathable Clothes: By providing a more comfortable environment for irritated vaginal tissue, loose-fitting clothing and cotton underwear can help manage the symptoms of bacterial vaginal lining infection (BV) or yeast infection.
7. Temporarily Abstain from Sexual Activity: Until therapy is finished, abstaining from sexual activity or wearing condoms can help stop the spread of new bacteria and promote healing.
8. Steer clear of Vaginal Irritants: Wipe from front to back, use gentle, unscented soaps, stay away from tampons and menstrual cups, and never spray.
Hydrogen Peroxide is the one to skip. Although some research indicates hydrogen peroxide may help with bacterial vaginosis symptoms, Gersh and Trubow advise against using it since it can be very harsh and destroy good bacteria.
In conclusion, breathable clothes, probiotic supplements, a diet high in nutrients, suppositories containing boric acid or tea tree oil, breathable garments, and a brief cessation of intercourse are all natural treatments for bacterial vaginosis. Steer clear of hydrogen peroxide and try to avoid vaginal irritants.
The Bottom Line: An imbalance in vaginal bacteria is the source of the frequent illness known as BV. It can be difficult to find the correct treatment, but more and more functional and integrative physicians are turning to natural therapies. Always speak with your physician to find the best course of action for your unique situation; for best outcomes, this may involve combining natural remedies with antibiotics.
Leave a Reply